Abstract
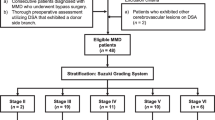
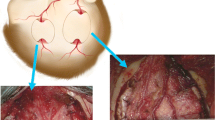
Direct bypass surgery improves blood flow in patients with moyamoya disease (MMD) as well as causes local flow relocation and disturbance. This study aimed to describe the characteristics and changes of quantitative blood flow in MMD patients. Sixty-four consecutive MMD patients (67 hemispheres) who underwent STA-MCA anastomosis between August 2013 and September 2017 were included in this study. Intraoperative blood flow of superficial temporal artery and middle cerebral artery was measured with a noninvasive, ultrasound flowprobe, before and after the bypass. All data were collected prospectively. Before the bypass, 67 hemispheres were measured and 45 hemispheres acquired post-bypass measurements. Thirty-three (49.3%) had anterograde flow and 34 (50.7%) had retrograde. Retrograde blood flow was significantly higher than anterograde blood flow in MCA-M4 section (3.71 ± 2.78 ml/min vs 2.39 ± 1.71 ml/min, P = 0.023). Thirty-eight (56.7%) patients had local cerebrovascular reactivity, whereas 29 (43.3%) lost it. After bypass, blood flow was changed into three patterns: anterograde flow (1, 2.2%), retrograde flow (3, 6.7%), and bi-direction flow (41, 91.1%). Flow of M4 was significantly improved in both proximal (13.64 ± 9.16 vs 3.28 ± 2.57, P < 0.001) and distal (7.17 ± 7.21 vs 3.28 ± 2.57, P = 0.002) sides to the bypass. Postoperative infarctions occurred in 4 (8.9%) patients. All postoperative infarctions (n = 4) happened in those patients who did not have change of flow direction in M4 section distal to the bypass (P = 0.040). Direct bypass surgery improves local blood flow after bypass surgery in both sides of the anastomosis. Flow direction was usually changed after the surgery into a bi-direction pattern: anterograde flow in M4 distal to the bypass, and retrograde flow in M4 proximal to the bypass. Proximal side acquired around 5.4 times of flow than the distal side. Patients with change of flow direction in distal M4 were related with lower risks of postoperative infarctions.




Similar content being viewed by others
References
Amin-Hanjani S, Du X, Mlinarevich N, Meglio G, Zhao M, Charbel FT (2005) The cut flow index: an intraoperative predictor of the success of extracranial-intracranial bypass for occlusive cerebrovascular disease. Neurosurgery 56:75–85 discussion 75-85
Bothun ML, Haaland OA, Logallo N, Svendsen F, Thomassen L, Helland CA (2016) Cerebrovascular reactivity after treatment of unruptured intracranial aneurysms--a transcranial Doppler sonography and acetazolamide study. J Neurol Sci 363:97–103. https://doi.org/10.1016/j.jns.2015.12.024
Bothun ML, Haaland OA, Logallo N, Svendsen F, Thomassen L, Helland CA (2018) Time course of cerebrovascular reactivity in patients treated for unruptured intracranial aneurysms: a one-year transcranial Doppler and acetazolamide follow-up study. Biomed Res Int 2018:6489276–6489279. https://doi.org/10.1155/2018/6489276
Charbel FT, Hoffman WE, Misra M, Ostergren L (1998) Ultrasonic perivascular flow probe: technique and application in neurosurgery. Neurol Res 20:439–442
Cho WS, Kim JE, Kim CH, Ban SP, Kang HS, Son YJ, Bang JS, Sohn CH, Paeng JC, Oh CW (2014) Long-term outcomes after combined revascularization surgery in adult moyamoya disease. Stroke 45:3025–3031. https://doi.org/10.1161/STROKEAHA.114.005624
Fujimura M, Tominaga T (2019) Hemorrhagic moyamoya disease : a recent update. J Korean Neurosurg Soc 62:136–143. https://doi.org/10.3340/jkns.2018.0101
Fujimura M, Mugikura S, Kaneta T, Shimizu H, Tominaga T (2009) Incidence and risk factors for symptomatic cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease. Surg Neurol 71:442–447. https://doi.org/10.1016/j.surneu.2008.02.031
Fujimura M, Bang OY, Kim JS (2016) Moyamoya disease. Front Neurol Neurosci 40:204–220. https://doi.org/10.1159/000448314
Han JS, Abou-Hamden A, Mandell DM, Poublanc J, Crawley AP, Fisher JA, Mikulis DJ, Tymianski M (2011) Impact of extracranial-intracranial bypass on cerebrovascular reactivity and clinical outcome in patients with symptomatic moyamoya vasculopathy. Stroke 42:3047–3054. https://doi.org/10.1161/STROKEAHA.111.615955
Januszewski J, Beecher JS, Chalif DJ, Dehdashti AR (2014) Flow-based evaluation of cerebral revascularization using near-infrared indocyanine green videoangiography. Neurosurg Focus 36:E14. https://doi.org/10.3171/2013.12.FOCUS13473
Kawamata T, Kawashima A, Yamaguchi K, Hori T, Okada Y (2011) Usefulness of intraoperative laser Doppler flowmetry and thermography to predict a risk of postoperative hyperperfusion after superficial temporal artery-middle cerebral artery bypass for moyamoya disease. Neurosurg Rev 34:355–362; discussion 362. https://doi.org/10.1007/s10143-011-0331-8
Kim JS (2016) Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke 18:2–11. https://doi.org/10.5853/jos.2015.01627
Kim DY, Son JP, Yeon JY, Kim GM, Kim JS, Hong SC, Bang OY (2017) Infarct pattern and collateral status in adult moyamoya disease: a multimodal magnetic resonance imaging study. Stroke 48:111–116. https://doi.org/10.1161/STROKEAHA.116.014529
Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurol 7:1056–1066. https://doi.org/10.1016/S1474-4422(08)70240-0
Lee M, Guzman R, Bell-Stephens T, Steinberg GK (2011) Intraoperative blood flow analysis of direct revascularization procedures in patients with moyamoya disease. J Cereb Blood Flow Metab 31:262–274. https://doi.org/10.1038/jcbfm.2010.85
Li X, Huang Z, Wu MX, Zhang D (2017) Effect of adventitial dissection of superficial temporal artery on the outcome of superficial temporal artery-middle cerebral artery bypass in moyamoya disease. Aging Dis 8:384–391. https://doi.org/10.14336/AD.2016.1115
Liu X, Zhang D, Shuo W, Zhao Y, Wang R, Zhao J (2013) Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J Neurol Neurosurg Psychiatry 84:258–265. https://doi.org/10.1136/jnnp-2012-302236
Lundell A, Bergqvist D, Mattsson E, Nilsson B (1993) Volume blood flow measurements with a transit time flowmeter: an in vivo and in vitro variability and validation study. Clin Physiol 13:547–557
Mazerolle EL, Ma Y, Sinclair D, Pike GB (2018) Impact of abnormal cerebrovascular reactivity on BOLD fMRI: a preliminary investigation of moyamoya disease. Clin Physiol Funct Imaging 38:87–92. https://doi.org/10.1111/cpf.12387
Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, Nakagawara J, Takahashi JC, Investigators JAMT (2014) Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke 45:1415–1421. https://doi.org/10.1161/STROKEAHA.113.004386
Morisawa H, Kawamata T, Kawashima A, Hayashi M, Yamaguchi K, Yoneyama T, Okada Y (2013) Hemodynamics and changes after STA-MCA anastomosis in moyamoya disease and atherosclerotic cerebrovascular disease measured by micro-Doppler ultrasonography. Neurosurg Rev 36:411–419. https://doi.org/10.1007/s10143-012-0441-y
Mukerji N, Cook DJ, Steinberg GK (2015) Is local hypoperfusion the reason for transient neurological deficits after STA-MCA bypass for moyamoya disease? J Neurosurg 122:90–94. https://doi.org/10.3171/2014.8.JNS132413
Nariai T, Matsushima Y, Imae S, Tanaka Y, Ishii K, Senda M, Ohno K (2005) Severe haemodynamic stress in selected subtypes of patients with moyamoya disease: a positron emission tomography study. J Neurol Neurosurg Psychiatry 76:663–669. https://doi.org/10.1136/jnnp.2003.025049
Okada Y, Shima T, Nishida M, Yamane K, Yamada T, Yamanaka C (1998) Effectiveness of superficial temporal artery-middle cerebral artery anastomosis in adult moyamoya disease: cerebral hemodynamics and clinical course in ischemic and hemorrhagic varieties. Stroke 29:625–630
Park SE, Kim JS, Park EK, Shim KW, Kim DS (2018) Direct versus indirect revascularization in the treatment of moyamoya disease. J Neurosurg 129:480–489. https://doi.org/10.3171/2017.5.JNS17353
Piao R, Oku N, Kitagawa K, Imaizumi M, Matsushita K, Yoshikawa T, Takasawa M, Osaki Y, Kimura Y, Kajimoto K, Hori M, Hatazawa J (2004) Cerebral hemodynamics and metabolism in adult moyamoya disease: comparison of angiographic collateral circulation. Ann Nucl Med 18:115–121
Research Committee on the P, Treatment of Spontaneous Occlusion of the Circle of W, Health Labour Sciences Research Grant for Research on Measures for Infractable D (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52:245–266
Sato S, Kojima D, Shimada Y, Yoshida J, Fujimato K, Fujiwara S, Kobayashi M, Kubo Y, Yoshida K, Terasaki K, Tsutsui S, Miyoshi K, Ogasawara K (2018) Preoperatively reduced cerebrovascular contractile reactivity to hypocapnia by hyperventilation is associated with cerebral hyperperfusion syndrome after arterial bypass surgery for adult patients with cerebral misery perfusion due to ischemic moyamoya disease. J Cereb Blood Flow Metab 38:1021–1031. https://doi.org/10.1177/0271678X18757621
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Tashiro R, Fujimura M, Kameyama M, Mugikura S, Endo H, Takeuchi Y, Tomata Y, Niizuma K, Tominaga T (2019) Incidence and risk factors of the watershed shift phenomenon after superficial temporal artery-middle cerebral artery anastomosis for adult moyamoya disease. Cerebrovasc Dis 47:178–187. https://doi.org/10.1159/000500802
Tu XK, Fujimura M, Rashad S, Mugikura S, Sakata H, Niizuma K, Tominaga T (2017) Uneven cerebral hemodynamic change as a cause of neurological deterioration in the acute stage after direct revascularization for moyamoya disease: cerebral hyperperfusion and remote ischemia caused by the ‘watershed shift’. Neurosurg Rev 40:507–512. https://doi.org/10.1007/s10143-017-0845-9
Uchino H, Nakayama N, Kazumata K, Kuroda S, Houkin K (2016) Edaravone reduces hyperperfusion-related neurological deficits in adult moyamoya disease: historical control study. Stroke 47:1930–1932. https://doi.org/10.1161/STROKEAHA.116.013304
Uda K, Araki Y, Muraoka S, Ota S, Wada K, Yokoyama K, Nishihori M, Izumi T, Okamoto S, Wakabayashi T (2018) Intraoperative evaluation of local cerebral hemodynamic change by indocyanine green videoangiography: prediction of incidence and duration of postoperative transient neurological events in patients with moyamoya disease. J Neurosurg 130:1–9. https://doi.org/10.3171/2017.10.JNS171523
Watchmaker JM, Juttukonda MR, Davis LT, Scott AO, Faraco CC, Gindville MC, Jordan LC, Cogswell PM, Jefferson AL, Kirshner HS, Donahue MJ (2018) Hemodynamic mechanisms underlying elevated oxygen extraction fraction (OEF) in moyamoya and sickle cell anemia patients. J Cereb Blood Flow Metab 38:1618–1630. https://doi.org/10.1177/0271678X16682509
Yamaguchi K, Kawamata T, Kawashima A, Hori T, Okada Y (2010) Incidence and predictive factors of cerebral hyperperfusion after extracranial-intracranial bypass for occlusive cerebrovascular diseases. Neurosurgery 67:1548–1554; discussion 1554. https://doi.org/10.1227/NEU.0b013e3181f8c554
Yun TJ, Paeng JC, Sohn CH, Kim JE, Kang HS, Yoon BW, Choi SH, Kim JH, Lee HY, Han MH, Zaharchuk G (2016) Monitoring cerebrovascular reactivity through the use of arterial spin labeling in patients with moyamoya disease. Radiology 278:205–213. https://doi.org/10.1148/radiol.2015141865
Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK (2011) Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke 42:2485–2491. https://doi.org/10.1161/STROKEAHA.111.616466
Funding
This study was funded by the Training Plan of High-level Technical Talents in Bei**g Health System (2015-3-041).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the institutional review board of Bei**g Tiantan Hospital, Capital Medical University, and Peking University International Hospital.
Informed consent
In accordance with the ethical decision, informed consent was obtained. No additional patient data collection or intervention was necessary. Furthermore, analysis was performed anonymized.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shi, G., Tan, C., Duan, R. et al. Intraoperative local hemodynamic quantitative analysis of direct revascularization in patients with moyamoya disease. Neurosurg Rev 44, 2659–2666 (2021). https://doi.org/10.1007/s10143-020-01442-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01442-9